
Managing diabetes effectively starts with choosing the right blood glucose monitoring system. In 2025, advancements in continuous glucose monitoring (CGM) technology have revolutionized diabetes care:
- Real-time tracking now helps patients maintain stable glucose levels.
- Integration with smartphones has increased patient engagement.
- Automated insulin delivery systems offer unprecedented convenience.
These innovations improve accuracy and reduce complications, empowering patients to take control of their health.
Key Takeaways
- Picking the best blood sugar monitor is important for managing diabetes. It can help you stay healthy and live better.
- Continuous glucose monitors (CGMs) show your sugar levels all the time. They help you keep your levels steady and avoid problems. These devices let you make smart choices for your health.
- Think about how accurate, simple, and affordable the monitor is. Easy-to-use devices make checking your sugar easier and more regular.
Why Choosing the Right Blood Glucose Monitoring System Matters
The role of accurate monitoring in diabetes management
Accurate blood glucose monitoring plays a pivotal role in managing diabetes effectively. It provides real-time insights into glucose levels, enabling patients to make informed decisions about their diet, exercise, and medication. Studies have shown that continuous glucose monitors (CGMs) reduce A1C levels by an average of 1.1%, compared to a 0.6% reduction with traditional methods. Additionally, CGMs increase the time spent in the target glucose range by 3.8 hours per day.
Smart blood glucose monitoring systems also contribute to better glycemic control. Research indicates that these systems lower mean blood glucose levels by 21.8 to 24.5 mg/dL, improving key metrics like fasting glucose and postprandial levels. These advancements minimize the risk of complications such as neuropathy, retinopathy, and cardiovascular disease.
| Study | Key Findings |
|---|---|
| Continuous Glucose Monitors | Reduced A1C by 1.1%; increased time in target glucose range by 3.8 hours/day |
| Smart Blood Glucose Monitoring | Lowered mean blood glucose by 21.8–24.5 mg/dL; improved glycemic metrics |
| Retrospective Study on CGM | A1C decreased from 11.21% to 7.04%; reduced hypoglycemic events significantly |
How the right system can improve quality of life
The right blood glucose monitoring system does more than track glucose levels—it transforms lives. For individuals with diabetes, CGMs have been linked to reduced time spent in hypoglycemia and increased time in the target glycemic range. Parents of children with diabetes report better sleep and reduced family stress when using CGMs with remote monitoring.
Moreover, these systems alleviate the fear of hypoglycemia, a common concern among adults with Type 1 diabetes. They also improve adherence to treatment plans and reduce psychosocial distress, particularly in younger patients. By offering real-time data and actionable insights, modern systems empower users to live more confidently and independently.
| Quality of Life Improvement | Evidence Source |
|---|---|
| Decreased time in hypoglycemia | 13 out of 15 studies in Type 1 diabetes show this effect from CGM usage. |
| Increased time in target glycemic range (TIR) | Observed in well-controlled patients with Type 1 diabetes using isCGM. |
| Reduced fear of hypoglycemia | Adult patients with Type 1 diabetes report perceived improvements in quality of life due to CGM. |
| Better quality of life for children | CGM with remote monitoring leads to improved parental sleep and reduced family stress. |
| Improved adherence and reduced psychosocial distress | Youth with Type 1 diabetes experience better adherence and lower psychosocial distress with CGM. |
Choosing the right blood glucose monitoring system is not just a medical decision—it’s a lifestyle upgrade. It bridges the gap between managing diabetes and living life to the fullest.
Key Factors to Consider When Choosing a Blood Glucose Monitoring System
Selecting the right blood glucose monitoring system involves evaluating several critical factors. Each aspect plays a vital role in ensuring effective diabetes management and improving the user experience.
Accuracy and reliability
Accuracy is the cornerstone of any blood glucose monitoring system. Without precise readings, users risk making incorrect decisions about their diet, medication, or insulin dosage. Clinical studies emphasize the importance of analytical accuracy. For instance, the American Diabetes Association recommends that systems maintain an analytical error of less than 10% for blood glucose levels between 30 and 400 mg/dL. Reducing this error to under 2% could lead to a 95% correct insulin dosing rate in ICU patients, underscoring the life-saving potential of accurate devices.
Comparative studies also highlight the reliability of various systems. For example:
| Study Title | Summary |
|---|---|
| Comparative Accuracy of 17 Point-of-Care Glucose Meters | Evaluates the performance of multiple glucose meters, offering insights into their reliability. |
| Accuracy and Reliability of Continuous Glucose Monitoring Systems | Discusses CGM accuracy, emphasizing the need for capillary blood glucose measurements before treatment decisions. |
When choosing a system, prioritize one with proven clinical accuracy and reliability to ensure optimal diabetes management.
Ease of use and user interface
A user-friendly design can make or break the experience of managing diabetes. Devices like the Dexcom G7 have set a new standard in usability. Older adults and diabetes educators have praised its simplicity, noting that it is easier to operate than previous models. The G7’s design incorporates feedback from diverse users, ensuring it meets the needs of both tech-savvy individuals and those less familiar with technology.
In regions with limited resources, usability becomes even more critical. Studies on prototype CGMs in low- and middle-income countries highlight the importance of intuitive interfaces to make these systems accessible to a broader audience. When evaluating a device, consider how easy it is to navigate menus, interpret data, and perform essential tasks like calibration.
Pro Tip: Look for systems with touchscreen displays or smartphone integration for a seamless user experience.
Cost and insurance coverage
Cost is a significant factor for many users. While continuous glucose monitoring systems offer advanced features, they often come with a higher price tag. However, cost-effectiveness analyses reveal that CGMs can reduce long-term healthcare expenses by improving glycemic control and reducing complications.
| Study | Findings | ICER (Cost per QALY) | Notes |
|---|---|---|---|
| Cost-effectiveness of CGM for Adults with T1D | CGM increased costs but reduced HbA1c and daily strip use | $98,108 | Robust results with sensitivity analyses; potential cost reduction with extended use |
| 17 studies | CGM is cost-effective | $42,000 to $175,000 | Majority of ICERs below GDP per capita thresholds for first-world countries |
Before purchasing, check your insurance coverage. Many plans now include CGMs, making them more affordable for patients.
Size, portability, and design
Portability is essential for users who are always on the go. Compact and lightweight devices fit seamlessly into daily life, allowing users to monitor their glucose levels discreetly. Modern systems prioritize sleek designs without compromising functionality. For example, wearable CGMs like the FreeStyle Libre 3 Plus are small enough to be worn comfortably for extended periods.
When selecting a device, consider its size and whether it aligns with your lifestyle. A portable system ensures that you can manage your diabetes effectively, no matter where you are.
Data tracking and smartphone compatibility
In 2025, data tracking has become a game-changer in diabetes management. Many blood glucose monitoring systems now sync with smartphones, offering features like:
- Continuous glucose monitoring
- Logging of fingerstick glucose values
- Tracking body weight and food intake
- Monitoring physical activity and estimating calories burned
- Accessing nutritional databases
These features provide a comprehensive view of your health, enabling better decision-making. Smartphone compatibility also allows users to share data with healthcare providers, ensuring personalized care.
Additional features like alarms and trend analysis
Advanced features can significantly enhance the functionality of a blood glucose monitoring system. Real-time alarms, for instance, alert users to high or low glucose levels, preventing dangerous situations. A multicenter study involving 254 adults with type 1 diabetes found that systems with alert functionality improved time in range and reduced HbA1c levels. Participants also reported fewer hypoglycemic episodes and greater satisfaction with their diabetes management.
Trend analysis is another valuable feature. By identifying patterns in glucose levels, users can anticipate fluctuations and adjust their routines accordingly. These tools empower individuals to take a proactive approach to their health.
Note: Systems with customizable alarms and detailed trend reports are particularly beneficial for users with a history of hypoglycemia.
Top Blood Glucose Monitoring Systems for 2025

Sejoy Blood Glucose Monitoring System: Features, pros, and cons
The Sejoy Blood Glucose Monitoring System stands out as a reliable and innovative choice for diabetes management in 2025. As a trusted name in healthcare, Sejoy has built its reputation on quality and technological excellence. This system offers exceptional accuracy, ensuring users can confidently manage their glucose levels. Its user-friendly design makes it accessible for individuals of all ages, while its compact size enhances portability.
Key features include:
- High accuracy and reliability: The system delivers precise readings, reducing the risk of incorrect insulin dosing.
- Smartphone compatibility: Seamless integration with mobile apps allows users to track and analyze their glucose data effortlessly.
- Affordable pricing: Sejoy offers a cost-effective solution without compromising on quality.
The Sejoy Blood Glucose Monitoring System combines innovation with practicality, making it a top contender for effective diabetes management.
Dexcom G7: Features, pros, and cons
The Dexcom G7 has redefined continuous glucose monitoring (CGM) with its cutting-edge technology. This system provides real-time glucose readings, empowering users to make informed decisions about their health. Its compact sensor and streamlined design ensure comfort and ease of use.
Key features include:
- Real-time monitoring: The G7 offers continuous glucose tracking, reducing the need for fingerstick tests.
- Customizable alerts: Users receive notifications for high or low glucose levels, enhancing safety.
- Smartphone integration: The system syncs with mobile devices, providing detailed glucose trends and insights.
However, user feedback highlights some challenges. For instance, 58% of respondents with type 2 diabetes reported variability in sensor accuracy, which affected their confidence in insulin dosing. Additionally, over 50% experienced skin reactions. Despite these concerns, the Dexcom G7 remains a popular choice for its advanced features and user-friendly interface.
FreeStyle Libre 3 Plus: Features, pros, and cons
The FreeStyle Libre 3 Plus continues to lead the market with its innovative approach to glucose monitoring. This system eliminates the need for routine fingersticks, offering a painless and convenient alternative. Its small, discreet sensor can be worn for up to 14 days, providing continuous glucose data.
Key features include:
- Compact design: The sensor is lightweight and comfortable, making it ideal for active users.
- Real-time data: Users can access their glucose levels instantly via a smartphone app.
- Trend analysis: The system identifies patterns, helping users optimize their diabetes management.
The FreeStyle Libre 3 Plus excels in portability and ease of use. It empowers users to take control of their health with minimal disruption to their daily lives.
OneTouch Verio Reflect: Features, pros, and cons
The OneTouch Verio Reflect offers a unique blend of simplicity and sophistication. Designed for individuals seeking a straightforward yet effective monitoring solution, this system provides accurate readings and actionable insights.
Key features include:
- Blood Sugar Mentor™ feature: Offers personalized guidance based on glucose trends.
- ColorSure® technology: Highlights when glucose levels are in or out of range.
- Bluetooth connectivity: Syncs with the OneTouch Reveal® app for data tracking and sharing.
The OneTouch Verio Reflect is an excellent choice for users who value clarity and guidance in their diabetes management journey. Its intuitive features make it a reliable companion for maintaining optimal glucose control.
CONTOUR NEXT ONE: Features, pros, and cons
The CONTOUR NEXT ONE sets a high standard for accuracy and convenience in blood glucose monitoring. This system boasts remarkable precision, with a mean relative bias of +2.2% and a coefficient of variation of 1.8%.
Key features include:
- Wireless connectivity: Bluetooth® integration allows seamless data transfer to the CONTOUR® Diabetes app.
- SmartLIGHT™ indicator: Provides instant feedback on glucose levels with color-coded alerts.
- Second-Chance® Sampling: Reduces test strip waste by allowing users to reapply blood within 60 seconds.
The CONTOUR NEXT ONE combines advanced technology with user-friendly features, making it a top choice for individuals seeking accuracy and efficiency in their diabetes management routine.
Emerging Technologies and Innovations in Blood Glucose Monitoring

Noninvasive glucose monitoring systems
Noninvasive glucose monitoring systems represent a groundbreaking shift in diabetes management. These systems eliminate the need for fingersticks, offering a painless and convenient alternative. Recent innovations include sensors that continuously monitor glucose levels without blood extraction, implantable systems requiring minimal calibration, and devices using infrared technology to measure glucose in interstitial fluid.
| Innovation | Description | Clinical Outcome |
|---|---|---|
| Non-invasive blood glucose sensors | Continuous monitoring without blood extraction | Improved blood sugar control and prevention of severe hypoglycemia |
| GlucoTrack’s implantable system | Long-term monitoring with minimal calibration | Accuracy of 3-9% MARD in clinical studies |
| DiaMonTech’s NIGM technology | Infrared beam targeting glucose in interstitial fluid | Painless and harmless measurement without consumables |
| Mini-NIR device | High accuracy in clinical testing | 95.6% of predicted values within acceptable error grid zones |
These advancements enhance the accuracy and accessibility of glucose monitoring, making it easier for users to manage their diabetes effectively.
Smartwatches and wearable devices
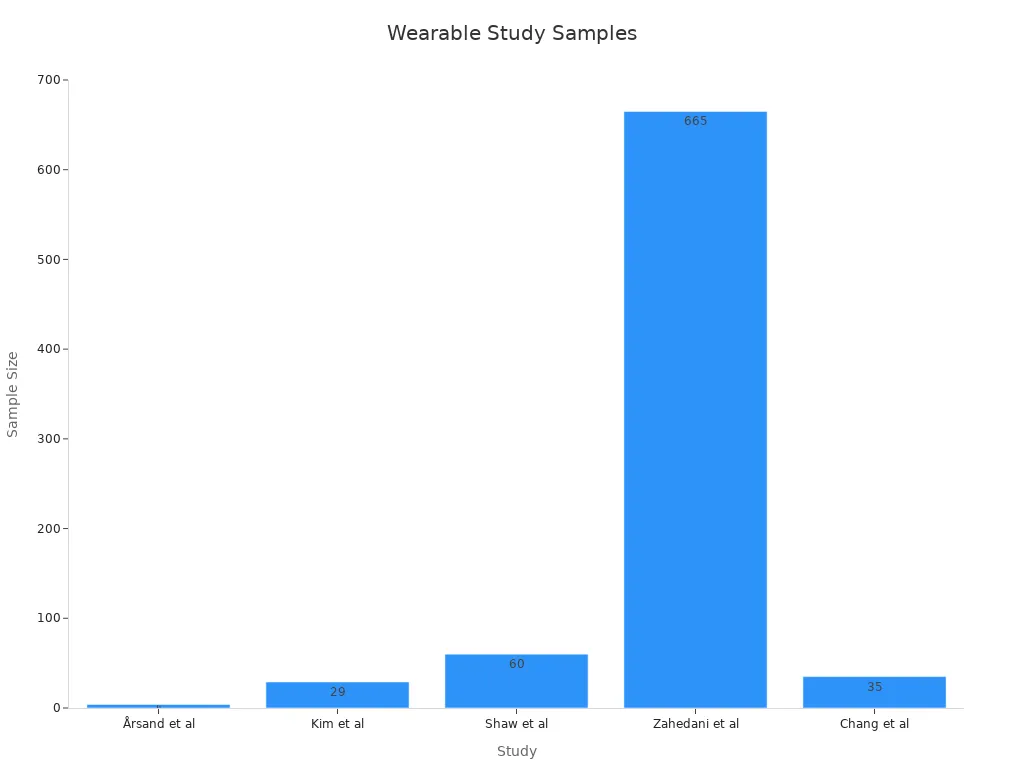
Smartwatches and wearable devices have transformed how we approach diabetes care. These tools integrate seamlessly into daily life, offering continuous glucose monitoring alongside features like activity tracking and dietary logging. Studies show that wearable devices improve adherence to treatment plans and encourage healthier lifestyles.
For example, a study by Kim et al. involving 29 adults with type 2 diabetes demonstrated a significant reduction in HbA1c levels after 12 weeks of using a smartphone-based diabetes care system. Similarly, Zahedani et al. found that combining continuous glucose monitoring with wearable devices improved time in range (TIR) by 22.7% in participants with poor glucose control.
These devices not only simplify glucose monitoring but also empower users to take a more proactive role in their health.
AI-powered glucose monitoring solutions
Artificial intelligence (AI) has revolutionized the capabilities of blood glucose monitoring systems. AI-powered devices analyze glucose data in real-time, providing tailored insulin dosage recommendations and reducing the need for invasive techniques.
- AI algorithms enhance the interpretation of continuous glucose monitoring (CGM) data, offering actionable insights for both patients and clinicians.
- Closed-loop systems integrate AI with insulin delivery, maintaining stable glucose levels more effectively than traditional methods.
- Literature reviews highlight the potential of AI to transform diabetes care by improving accuracy and personalization.
For instance, a study on AI-powered CGM devices demonstrated their ability to calculate insulin dosages accurately, reducing the risk of complications. These advancements make diabetes management more efficient and user-friendly, paving the way for a future where technology and healthcare work hand in hand.
Practical Tips for Effective Glucose Monitoring
Establishing a consistent monitoring routine
Consistency is key when managing diabetes effectively. I recommend setting clear, personalized goals for monitoring frequency and timing. For example, using SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound) can help you stay on track. Regularly reviewing your glucose data allows you to identify patterns, such as how your levels fluctuate throughout the day. This insight helps you make informed decisions about your diet and activity.
To minimize the burden of monitoring, choose a device that requires a small sample size and delivers fast results. Rotating testing sites can also reduce discomfort. Always wash your hands before testing to ensure accuracy, and avoid alternate sites unless your device is designed for them. If you notice unusual patterns or experience issues, don’t hesitate to contact your healthcare provider for guidance.
Understanding and interpreting glucose data
Interpreting glucose data can feel overwhelming, but it’s essential for effective diabetes management. Continuous glucose monitoring (CGM) systems, flash monitors, and self-monitoring blood glucose (SMBG) devices each offer unique insights. Studies show that CGM users achieve an interpretation accuracy of 38.0%, while flash monitors score slightly higher at 39.5%. SMBG devices, though less advanced, still provide valuable data with an accuracy rate of 33.3%.
| Monitoring Method | Interpretation Accuracy (%) | Treatment Action Accuracy (%) |
|---|---|---|
| CGM | 38.0 ± 11.1 | 21.5 ± 15.6 |
| Flash | 39.5 ± 8.8 | 21.2 ± 14.0 |
| SMBG | 33.3 ± 7.8 | 18.0 ± 13.2 |
Understanding these numbers helps you take appropriate actions, such as adjusting your insulin dosage or modifying your meals. Over time, you’ll become more confident in analyzing trends and making proactive decisions.
Maintaining and calibrating your device
Proper maintenance ensures your blood glucose monitoring system remains accurate and reliable. Regularly clean your device and check for any signs of wear or damage. If your system requires calibration, follow the manufacturer’s instructions carefully. For example, some devices need periodic coding to maintain accuracy.
Battery life is another critical factor. Always keep spare batteries or a charger on hand, especially if you rely on your device throughout the day. By taking these steps, you can extend the lifespan of your system and ensure consistent performance.
Tips for traveling with a glucose monitoring system
Traveling with a blood glucose monitoring system requires careful planning. Start by packing extra supplies, including test strips, lancets, and batteries. Keep these items in your carry-on bag to ensure easy access during your journey.
When flying, inform security personnel about your device to avoid delays during screening. Many modern systems, like CGMs, are compatible with smartphones, making it easier to monitor your levels on the go. If you’re traveling across time zones, adjust your monitoring schedule to align with local time.
Pro Tip: Always carry a letter from your healthcare provider explaining your condition and the need for your device. This can be helpful in emergencies or when navigating airport security.
Selecting the right blood glucose monitoring system is crucial for effective diabetes management. Advanced technologies improve glycemic control and enhance psychological well-being for patients with type 1 and type 2 diabetes. However, disparities in access to these tools can worsen health inequities. Factors like cost and prescribing practices often limit equitable use.
The Sejoy Blood Glucose Monitoring System stands out for its innovation and reliability. Its user-friendly design and accurate readings empower patients to manage their health confidently. I recommend evaluating your lifestyle and consulting healthcare professionals to find the system that best aligns with your needs.
FAQ
What is the most accurate blood glucose monitoring system in 2025?
The Sejoy Blood Glucose Monitoring System offers exceptional accuracy, ensuring reliable readings for effective diabetes management. Its advanced technology minimizes errors and supports confident decision-making.
Can I use a blood glucose monitoring system without a smartphone?
Yes, many systems, including the Sejoy device, function independently. However, smartphone integration enhances data tracking and analysis for a more comprehensive experience.
How often should I calibrate my blood glucose monitoring device?
Calibration frequency depends on the device. Some systems, like the Sejoy model, require minimal or no calibration, simplifying maintenance and ensuring consistent accuracy.
Pro Tip: Always follow the manufacturer’s guidelines for calibration and maintenance to maximize your device’s performance.
Post time: May-30-2025

